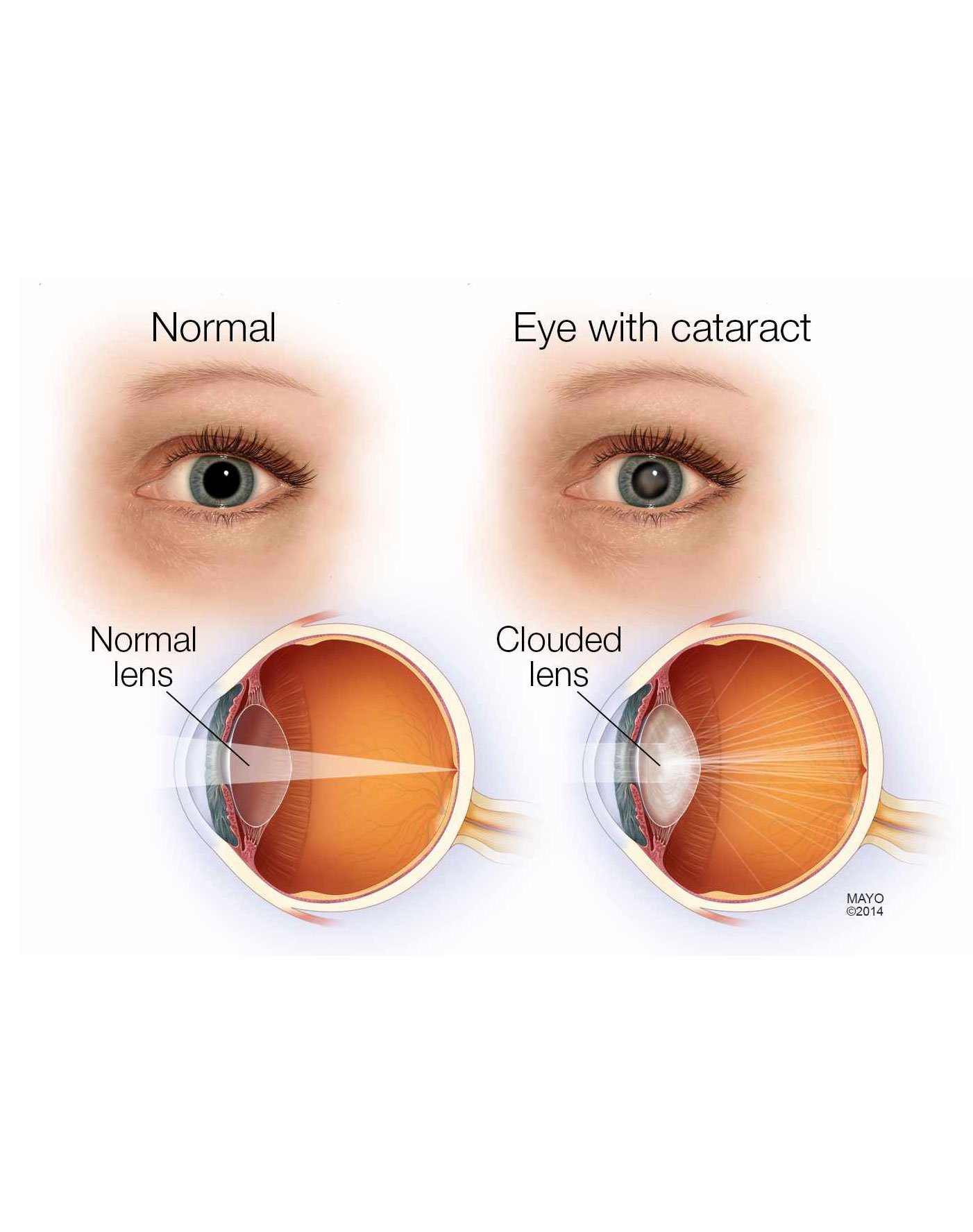
A cataract is a clouding of the lens in the eye which leads to a decrease in vision. Cataracts often develop slowly and can affect one or both eyes. Symptoms may include faded colors, blurry vision, halos around light, trouble with bright lights, and trouble seeing at night. This may result in trouble driving, reading, or recognizing faces. Poor vision caused by cataracts may also result in an increased risk of falling and depression. Cataracts cause half of all cases of blindness and 33% of visual impairment worldwide.
Cataracts are most commonly due to aging but may also occur due to trauma or radiation exposure, be present from birth, or occur following eye surgery for other problems. Risk factors include diabetes, smoking tobacco, prolonged exposure to sunlight, and alcohol. The underlying mechanism involves accumulation of clumps of protein or yellow-brown pigment in the lens that reduces transmission of light to the retina at the back of the eye. Diagnosis is by an eye examination.
Prevention includes wearing sunglasses and not smoking. Early on the symptoms may be improved with glasses. If this does not help, surgery to remove the cloudy lens and replace it with an artificial lens is the only effective treatment. Surgery is needed only if the cataracts are causing problems and generally results in an improved quality of life. Cataract surgery is not readily available in many countries, which is especially true for women, those living in rural areas, and those who do not know how to read.
About 20 million people are blind due to cataracts. It is the cause of approximately 5% of blindness in the United States and nearly 60% of blindness in parts of Africa and South America. Blindness from cataracts occurs in about 10 to 40 per 100,000 children in the developing world, and 1 to 4 per 100,000 children in the developed world. Cataracts become more common with age. More than half the people in the United States had cataracts by the age of 80.
Causes
Age
Age is the most common cause. Lens proteins denature and degrade over time, and this process is accelerated by diseases such as diabetes mellitus and hypertension. Environmental factors, including toxins, radiation, and ultraviolet light, have cumulative effects, which are worsened by the loss of protective and restorative mechanisms due to alterations in gene expression and chemical processes within the eye.
Trauma
Post traumatic rosette cataract of a 60-year-old male
Blunt trauma causes swelling, thickening, and whitening of the lens fibers. While the swelling normally resolves with time, the white color may remain. In severe blunt trauma, or in injuries that penetrate the eye, the capsule in which the lens sits can be damaged. This damage allows fluid from other parts of the eye to rapidly enter the lens leading to swelling and then whitening, obstructing light from reaching the retina at the back of the eye. Cataracts may develop in 0.7 to 8.0% of cases following electrical injuries.[13] Blunt trauma can also result in star- or petal-shaped cataracts.
Radiation
Cataracts can arise as an effect of exposure to various types of radiation. X-rays, one form of ionizing radiation, may damage the DNA of lens cells.[15] Ultraviolet light, specifically UVB, has also been shown to cause cataracts, and some evidence indicates sunglasses worn at an early age can slow its development in later life. Microwaves , a type of nonionizing radiation, may cause harm by denaturing protective enzymes (e.g., glutathione peroxidase), by oxidizing protein thiol groups (causing protein aggregation), or by damaging lens cells via thermoelastic expansion.[15] The protein coagulation caused by electric and heat injuries whitens the lens. This same process is what makes the clear albumen of an egg become white and opaque during cooking.
Genetics
Christmas tree cataract (Diffuse illumination)
The genetic component is strong in the development of cataracts, most commonly through mechanisms that protect and maintain the lens. The presence of cataracts in childhood or early life can occasionally be due to a particular syndrome. Examples of chromosome abnormalities associated with cataracts include 1q21.1 deletion syndrome, cri-du-chat syndrome, Down syndrome, Patau's syndrome, trisomy 18 (Edward's syndrome), and Turner's syndrome, and in the case of neurofibromatosis type 2, juvenile cataract on one or both sides may be noted. Examples of single-gene disorder include Alport's syndrome, Conradi's syndrome, cerebrotendineous xanthomatosis, myotonic dystrophy, and oculocerebrorenal syndrome or Lowe syndrome.
Signs and symptoms:
Signs and symptoms vary depending on the type of cataract, though considerable overlap occurs. People with nuclear sclerotic or brunescent cataracts often notice a reduction of vision. Those with posterior subcapsular cataracts usually complain of glare as their major symptom.
The severity of cataract formation, assuming no other eye disease is present, is judged primarily by a visual acuity test. Other symptoms include frequent changes of glasses and colored halos due to hydration of lens.
Skin diseases
The skin and the lens have the same embryological origin and so can be affected by similar diseases. Those with atopic dermatitis and eczema occasionally develop shield ulcer cataracts. Ichthyosis is an autosomal recessive disorder associated with cuneiform cataracts and nuclear sclerosis. Basal-cell nevus and pemphigus have similar associations.
Prevention
Risk factors such as UVB exposure and smoking can be addressed. Although no means of preventing cataracts has been scientifically proven, wearing sunglasses that counteract ultraviolet light may slow their development. While adequate intake of antioxidants (such as vitamins A, C, and E) has been thought to protect against the risk of cataracts, clinical trials have shown no benefit from supplements;[22] though evidence is mixed, but weakly positive, for a potential protective effect of the nutrients lutein and zeaxanthin. Statin use is somewhat associated with a lower risk of nuclear sclerotic cataracts.
Treatment
Surgical
Main article: Cataract surgery
Cataract surgery, using a temporal-approach phacoemulsification probe (in right hand) and "chopper" (in left hand) being done under operating microscope at a navy medical center
Slit lamp photo of posterior capsular opacification visible a few months after implantation of intraocular lens in eye, seen on retroillumination
The appropriateness of surgery depends on a person's particular functional and visual needs and other risk factors. Cataract removal can be performed at any stage and no longer requires ripening of the lens. Surgery is usually 'outpatient' and usually performed using local anesthesia. About 9 of 10 patients can achieve a corrected vision of 20/40 or better after surgery.
Several recent evaluations found that cataract surgery can meet expectations only when significant functional impairment due to cataracts exists before surgery. Visual function estimates such as VF-14 have been found to give more realistic estimates than visual acuity testing alone. In some developed countries, a trend to overuse cataract surgery has been noted, which may lead to disappointing results.
Phacoemulsification is the most widely used cataract surgery in the developed world. This procedure uses ultrasonic energy to emulsify the cataract lens. Phacoemulsification typically comprises six steps:
Anaesthetic – The eye is numbed with either a subtenon injection around the eye (see: retrobulbar block) or topical anesthetic eye drops. The former also provides paralysis of the eye muscles.
Corneal incision – Two cuts are made at the margin of the clear cornea to allow insertion of instruments into the eye.
Capsulorhexis – A needle or small pair of forceps is used to create a circular hole in the capsule in which the lens sits.
Phacoemulsification – A handheld ultrasonic probe is used to break up and emulsify the lens into liquid using the energy of ultrasound waves. The resulting 'emulsion' is sucked away.
Irrigation and aspiration – The cortex, which is the soft outer layer of the cataract, is aspirated or sucked away. Fluid removed is continually replaced with a saline solution to prevent collapse of the structure of the anterior chamber (the front part of the eye).
Lens insertion – A plastic, foldable lens is inserted into the capsular bag that formerly contained the natural lens. Some surgeons also inject an antibiotic into the eye to reduce the risk of infection. The final step is to inject salt water into the corneal wounds to cause the area to swell and seal the incision.
Extracapsular cataract extraction (ECCE) consists of removing the lens manually, but leaving the majority of the capsule intact.[48] The lens is expressed through a 10- to 12-mm incision which is closed with sutures at the end of surgery. ECCE is less frequently performed than phacoemulsification, but can be useful when dealing with very hard cataracts or other situations where emulsification is problematic. Manual small incision cataract surgery (MSICS) has evolved from ECCE. In MSICS, the lens is removed through a self-sealing scleral tunnel wound in the sclera which, ideally, is watertight and does not require suturing. Although "small", the incision is still markedly larger than the portal in phacoemulsion. This surgery is increasingly popular in the developing world where access to phacoemulsification is still limited.
Intracapsular cataract extraction (ICCE) is rarely performed.[49] The lens and surrounding capsule are removed in one piece through a large incision while pressure is applied to the vitreous membrane. The surgery has a high rate of complications.